Community Health Workers and their Role in Diabetes Disease Management
 Chronics conditions, like diabetes, continue to affect the public, yet optimal preventative care and treatment is not secured for the many communities. Many individuals face lack of access to quality, culturally appropriate preventative healthcare. Diabetes self-management education is considered a very important component of diabetes care. However many individuals do not receive self-management training or they receive interventions that are not effective.
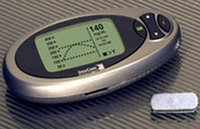
Chronics conditions, like diabetes, continue to affect the public, yet optimal preventative care and treatment is not secured for the many communities. Many individuals face lack of access to quality, culturally appropriate preventative healthcare. Diabetes self-management education is considered a very important component of diabetes care. However many individuals do not receive self-management training or they receive interventions that are not effective.As seen in previous blogs, healthcare is moving towards implementation of new media to breakdown some of the barriers faced in despaired communities. Access to technology can begin to bridge a gap between the digital divide, but who or what will connect the patient to the provider once they have access to the services?
Community Health Workers (CHWs) are defined as community members who work in community settings and serve as connectors between consumers and providers to promote health among groups that have traditionally lacked access to adequate healthcare. They are often referred to as the ‘vital links’ or the ‘in-between people.’ In my opinion, these individuals are a necessity for successful management programs. They can provide the support needed to gain skills for self-management. As a community member, the CHW is often seen as a peer rather than a provider.
A successful, integrated CHW-based diabetes program at Gateway Community Health Center in Laredo, TX recognized the need for additional assistance to address escalating health disparities and implemented Amigos en Salud, a program developed in partnership with Pfizer Health Solutions, which trains CHWs to educate Hispanics with diabetes to develop and maintain self-management skills and behavior change. CHWs support patients by providing a culturally relevant education curriculum, connecting patients and their families to the healthcare system and available community resources. The skills and responsibilities of CHWs from this program have been successfully woven into clinic operations, complementing the efforts of clinical and non-clinical staff. CHWs work in conjunction with the healthcare team, reinforcing and simplifying provider’s treatment plan in areas such as nutritional counseling, ensuring appointment keeping and participation in clinic programs. This CHW model enhances patient, family members and provider continuity and coordination of care, while increasing the delivery of quality care in the clinic. CHW insights into achieving clinic support, strategies for successful implementation and suggestions for overcoming obstacles will be discussed.
Integrating Internet with disease management and the support given by a CHW can only enhance the healthcare delivery in communities facing disparities. In order to incorporate new media into healthcare delivery, public health must continue its expansion as well. Individuals in the field must become part of the Internet community in order to continue building new neighborhoods.