Influence of the Internet on Diabetes Disease Management
Introduction
Digital information technology and electronic media are transforming individual and community health. This new media is affecting lifestyles, social institutions, and public policy. Health education and prevention programs are utilizing the new media to empower the patient. This technology revolution can bring tremendous benefits to individuals with chronic conditions participating in disease management programs.
The United States has experienced a dramatic increase in chronic conditions and by 2030, almost half of all Americans will have at least one chronic condition. A chronic condition that has been recognized as an important public health concern is diabetes. With more than 14 million people in the United States diagnosed with diabetes, it is the fifth leading cause of death in the United States. Diabetes can lead to numerous negative health outcomes such as heart attacks, stroke, kidney failure, nerve damage, and blindness. Though these are the facts, many individuals with diabetes do not receive the care needed to reduce risk of complications because the healthcare delivery system in this country is concentrated in acute care services. Quality improvement programs should emphasize the importance of treating diabetic patients for hypertension and controlling other major cardiovascular disease risk factors, such as smoking, dyslipidemia, and obesity, that are prevalent among these high-risk patients. According to the American Diabetes Association, the cost of care and complications of diabetes exceeds $132 billion annually. Although there is no cure for diabetes, early detection, lifestyle changes, and medication may serve to control the disease and reduce life-threatening complications. New media can allow patients to manage their diabetes, allowing them to gain control of their health. It can also assist in alleviating the pressures professionals face and aid in multi-tasking, which would improve the healthcare delivery system.
Diabetes
Diabetes is a set of related diseases in which blood glucose levels are above normal. Glucose, produced by the liver and released into the blood, provides the body with energy to perform daily functions. Produced by the pancreas, insulin regulates the blood glucose level. Insulin and glucagon are secreted from the pancreas in response to blood sugar levels, but as demonstrated in the picture their methods for controlling normal blood sugar are reverse. The pancreas has a crucial role in determining if a patient has diabetes, hypoglycemia, or other sugar problems. Insulin allows glucose to move from the blood into liver, muscle, and fat cells, where it is used for fuel. People with diabetes either do not produce enough insulin (type 1 diabetes) or cannot use insulin properly (type 2 diabetes), or both.
In diabetes, glucose in the blood cannot move into cells, and it stays in the blood. The increased level of blood glucose harms the cells that need the glucose for fuel and damages certain organs and tissues exposed to the high glucose levels; increasing the risk of several other conditions, the most important being heart disease (the number one leading cause of death). It is important to note that there are two major types of diabetes, type 1 and type 2.
Diabetes type 1 occurs when beta cells have been destroyed and no insulin or a small amount of insulin is produced. The lack of insulin results in increased blood glucose, a breakdown of lipids for energy and a depletion of protein. The inability to use the glucose in the bloodstream increases hunger and causes the patient to urinate more, which in turn causes excessive thirst. Type 1 diabetes can occur at any age, but it usually starts in people younger than 30. Symptoms are usually severe and occur rapidly. The exact cause of type 1 diabetes is not known. Type 1 is often referred to as juvenile or insulin-dependent diabetes.
Ninety percent of individuals diagnosed with diabetes have type 2. Diabetes type 2 appears without the classic warnings of diabetes. It generally occurs after the age of 30 and is often related to obesity. This form of diabetes is often controlled through diet, weight loss, and exercise, but when lifestyle changes are not completely effective, oral medications are added to the regimen. The primary metabolic process that contributes to diabetes type 2 is insulin resistance. As insulin resistance develops, the circulating glucose is not transported into the cells, which then triggers increased insulin secretion from beta cells. Hyperinsulinemia, excess levels of circulating insulin in the blood, is one of the first signs of insulin resistance.
According to the Center for Disease Control and Prevention (CDC) rates of diabetes have been linked to the increase in obesity in the United States. Children are now being diagnosed with diabetes type 2, a condition once only affecting individuals over the age of 30. A study conducted by the CDC found that from 1990 to 1998, diabetes rose 33% among U.S. adults and rates of type 2 diabetes rose another 6% among adults in 1999.
Pre-diabetes is often a precursor to diabetes type 2. The blood glucose levels of individuals with pre-diabetes are higher than normal, but not yet high enough to be diagnosed as diabetes. In the United States there are over 40 million people, ages 40 to 74, with have pre-diabetes. Pre-diabetes is a relatively new clinical diagnosis. In the past the condition was referred to as impaired glucose tolerance, but by renaming it pre-diabetes it highlights the seriousness of the condition and motivates people to seek appropriate treatment. Through early intervention methods to manage your blood glucose, individuals with pre-diabetes can delay or prevent type 2 diabetes from developing.
Along with early detection and treatment, control of glycemia, lipids, and hypertension can effectively delay or prevent diabetes complications. Many of these treatments are cost-effective, yet their implementation in the United States remains minimal and inconsistent. There is considerable pressure on U.S. healthcare systems to improve this situation and to deliver high-quality care while controlling costs. Though the Diabetes Quality Improvement Project (DQIP) was designed to influence the care of patients with diabetes, studies have demonstrated the substantial gap between the recommended diabetes care and the care patients are actually receiving in the United States. A particular study on diabetics found that 18.9% of the participants had a hemoglobin A1c (HbA1c) level greater than 9.5% (normal being between 4-6%), 58.0% had poor lipid control, 34.3% had poor blood pressure control, 36.7% did not receive an annual dilated eye examination, and 45.2% did not have a foot examination. Diabetes care in the United States can be vastly improved, and such improvement may yield substantial health benefits.
Disease Management Programs
Though beneficial, primary care providers have been hesitant to implement patient care guidelines and recommendations. Several barriers to guideline implementation include the perception that type 2 diabetes is not a serious condition, that aggressive treatment cannot prevent complications, that guidelines are not flexible enough to be useful in patient care, and that patients with diabetes are unwilling to make needed lifestyle changes. Given the rise of individuals with the condition and economic burden to society, improving care for patients with diabetes has become a major public health concern. The number and complexity of services required to manage patients with diabetes has made this population the target of multiple disease management efforts, as well as professional education and case management initiatives.
Disease management programs (DMPs) are a measure proposed to address the wide practice variations in healthcare delivery. Key elements of a Disease management program are:
multiprofessional, multidisciplinary, acute care, prevention and health promotion
Integrated care, care continuum, coordination of the different components
Population orientation (defined by a specific condition)
Active client-patient management tools (health education, empowerment, self-care)
Evidence-based guidelines, protocols, care pathways
Information technology, system solutions
Continuous quality improvement
Through disease management one can coordinate care, focusing on the whole clinical course of a disease. Services are organized and delivered according to scientific evidence and patients are actively involved in order to achieve better health outcomes. Investing in DMPs may be expensive; therefore it is important to study the cost-effectiveness of any DMP before introducing it to a system.
Diabetes DMPs can be an effective tool in contolling glycemic levels. They can reasonably improve glycemic control and can increase screening for retinopathy and foot complications. Studies have also shown that DMPs may improve quality of life and are potentially cost-effective. In order to find which DMP can lead to optimal health outcomes several factors need to be assessed including characteristics of the local health services, patient population, barriers to the access to optimal medical care, social and economic resources.
Cost of DMPs can be a barrier to implementation for many facilities, but adapting appropriate program can not only be both cost-effective and cost-saving.
Internet and DMPs
Self-management programs with the guidance of physicians and allied health professions can also help facilitate the care diabetic patients need. Care management is a means of providing easier, time-efficient communication between providers and patients, while improving care and reducing healthcare costs. Due to the increased accessibility, rates of patients accessing medical content on the Internet are also rising. In a survey of patients in a primary care practice, 54% of participants reported using the Internet for medical information and 60% felt that the information was the same or better than what they received from their doctor. Since scheduling and/or travel methods are often barriers faced by patients seeking healthcare services, diabetes care management utilizing a web-based system in individuals with poorly controlled diabetes can result in a significant and sustained improvement in HbA1c and blood pressure. Through the use of web-based health education significant improvements in HbA1c among patient with diabetes can be seen. Electronic databases can also expedite the availability of medical records. Though debatable there has been cost-savings with the implementation of both DMPs and care management in diabetes. Studies show the effectiveness of care management, particularly among individuals interested in engaging with the technology. Several major advantages in using web-based care management programs have been pointed out, including the ability to post professionally examined material on secure websites, 24-hour accessibility, and availability to individuals in their home. The Internet has clearly become the gateway to limitless health information; however support is lacking reguarding the clinical benefit of using web-based education and/or healthcare provider feedback.
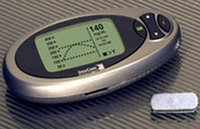
Internet-based blood glucose monitoring systems (IBGMSs) can allow patients to maintain steady levels of glucose and improved the degree of their glucose control. The Internet helps provide the stimulation and motivation needed for diabetics to control glucose levels. Originally focused on emotional support, Internet disease management programs for diabetes provide information to engage patients, allow the growth for self-management and counseling. Studies have shown that online services are as effective as face-to-face guidance and treatment in managing diabetes. The IBGMS have the potential for developing into advanced networking systems, which would allow close communication between the physician at the network center and the patient at their personal computer. One way to facilitate this would be through wireless devices, which could allow the providers to send test results immediately. Internet-based self-management interventions have great potential to enhance the care of diabetes and other chronic conditions. Greater attention must be focused on methods to maintain longitudinal involvement with Internet-based intervention health promotion programs.
The World Wide Web has became an essential tool in education, government, business, news media, medicine and research. Initially designed as an emergency communications network, the Internet has had an astonishing growth of over 250 million domains and hosts. Under ideal circumstances, the Internet can be very cost-effective, but as already reiterated, supporting the cost-effectiveness of management programs has not been an easy task and debate continues. Though modern technology can facilitate communication between providers and patients who are remotely separated, physicians will continue to be reluctant to accept this method on interacting with their patients until they can be compensated for eHealth.
EHealth is more suited for managed care programs, where health care providers are receiving a fixed salary. There are legal issues that will need to be considered for cyber encounters with patients, relative to how much patient history and data the physician is expected to store in the physician’s hospital or heath plan computer system and how easy it is to access this information in an emergency.
The Internet can be a resource for social support. Participation in disease-specific online communities have been growing in recent years. Many individuals venture the Internet and join support groups where they can communicate with peers and share their own experiences; providing support and advice to members of their online community.
Surveys have found that 80%of all patients go online for health-related information and of those on-line, 90% said the information on the web improved their understanding of their health conditions. The use of the Internet as a tool for Health promotion is crucials as 70% of chronic disease and early death are believed to be preventable through lifestyle changes. Forty-six percent of health consumers prefer to get their health information from the web rather than from their doctor. One-third of the patients going online actually take the information found to their providers, validating the empowering effect of the Internet on the patient. Studies have establish that use of computers and the Internet improves communication between youth and adults, raises perception of social status, increases participation within the community, supports reflective thought, increased efficiency, and improves access to resources.
Researchers, both formal and informal, are taking advantage of new media. Compared with traditional media, interactive health communication offers numerous advantages. These advantages include tailoring information to the specific needs of a population, protecting the anonymity of the user, and enhancing the ability to update and maintain current scientific knowledge; but there are obstacles faced by the informal researcher, the patient. One major barrier that needs further examination is the lack of new media literacy. Without the skills needed to utilize the Internet, individuals lack the motivation to empower themselves via new media. Through the use of appropriate interventions, multimedia users with low-literacy can gain in knowledge, self-efficacy, and perceived susceptibility to complications.
The ability of the Internet to facilitate quick exchange of information to large, geographically dispersed audience has greatly transformed health education and healthcare delivery. It has increased the efficacy of patient care by allowing instant and collaborative communication in a virtual global community. The Internet provides easy access to information on health and disease topics, drugs, and research findings. In addition, health professionals, local communities, and government agencies increasingly use the Internet for both disease prevention and to promote the overall health of the population.
Concusion
As rates of diabetes continue to affect populations, disease management programs must be integrated into healthcare delivery systems. Internet-based disease management systems for chronic conditions are becoming more popular. Though the cost-effectiveness of these systems is debatable, the benefits are unquestionable. The early dectection and treatment of diabetes can reduce the risks of severe complications. The Internet can play an influential role in early detection and treatment of diabetes and can encourage individual and community behavior changes.
Internet technology has made it possible to surpass the traditional face-to-face treatment for diabetes management, yet patients and providers utilizing new media face numerous barriers. Guidelines and regulations need to be established that govern the online communication between patient and provider, the quality of information available online must be monitored and regulated, and increasing accessibility to the Internet must be made a priority for all communities. A major goal of Health People 2010 is to implement new tools and strategies that will eliminate health disparities among low-income Americians and minorities. The Internet has the potential to improve the health of these communities. Increasing Internet accessibility and further developing telemedicine and eHealth will improve healthcare practive and delivery, as well as provide social and economic benefits to society.
Additional Resources
American Diabetes Association
CDC on Diabetes Basics
National Diabetes Information Clearinghouse
Diabetic Gourmet
Alternative Diabetes Treatment
Health Message Boards
Diabetes Disease Management Blog
Diabetes Mine
References
Atkinson NL, Gold RS. The Promise and Challenge of eHealth Interventions. The American Journal of Health Behavior. 2005; 26(2): 494-503.
Gerber BS, Brodsky IG, Lawless KA, Smolin LI, Arozullah AM, Smith EV, et al. Implementation and Evaluation of a Low-Literacy Diabetes Education Computer Multimedia Application. Diabetes Care. 2005; 28(7): 1574-1580.
Godley PJ, Maue SK, Farrelly EW, Frech F. The Need for Improved Medical Management of Patients With Concomitant Hypertension and Type 2 Diabetes Mellitus. The American Journal of Managed Care. 2005; 11(4): 206-210.
Karter AJ, Moffet HH, Liu J, MS; Parker MM, Ahmed AT, Ferrara A, Selby JV. Achieving Good Glycemic Control: Initiation of New Antihyperglycemic Therapies in Patients with Type 2 Diabetes From the Kaiser Permanente Northern California Diabetes Registry. The American Journal of Managed Care. 2005; 11(4): 262-270.
Knight K, Badamgarav E, Henning JM, Hasselblad V, Gano AD, Ofman JJ, et al. A Systematic Review of Diabetes Disease Management Programs. The American Journal of Managed Care. 2005; 11(4): 243-250.
Lahtela JT, Lamminen H: Telemedical Devices in Diabetes Management. Annals of Medicine. 2002; 34: 241–247.
Macias W, Lewis LS, Smith TL. Health-Related Message Boards/Chat Rooms on the Web: Discussion Content and Implications for Pharmaceutical Sponsorships. Journal of Health Communication. 2005; 10: 2009-2023.
McFarlane SI, Jacober SJ, Winer N. Control of Cardiovascular Risk Factors in Patients with Diabetes and Hypertension at Urban Academic Medical Centers. Diabetes Care. 2002; 25: 718-723.
McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The Diabetes Network Internet-Based Physical Activity Intervention. Diabetes Care. 2001; 24(8): 1328-1334.
McMahon GT, Gomes HE, Hickson S, Hu TM, Levine BA, Conlin PR. Web-Based Care Management in Patients With Poorly Controlled Diabetes. Diabetes Care, 2005; 28(7): 1624-1629.
Piette JD. The Future of Diabetes Disease Management: Integrating Lessons Learned from Clinical, Health Services, and Policy Research. The American Journal of Managed Care. 2005; 11(4): 203-205.
Roccaforte R, Demers C, Baldassarre F, Teo KK, Yusuf S.Effectiveness of Comprehensive Disease Management Programmes in Improving Clinical Outcomes: A meta-analysis. The European Journal of Heart Failure. 2005; 7:1133-44.
Rothman RL, So SA, Shin J, Malone RM, Bryant B, DeWalt DA. Labor Characteristics and Program Costs of a Successful Diabetes Disease Management Program. The American Journal Of Managed Care. 2006; 12(5): 277-283.
Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KV. A Diabetes Report Card for the United States: Quality of Care in the 1990s. Annals of Internal Medicine. 2002; 136(8): 565-574.
Turkoski BB. Diabetes and Diabetes Medications. Orthopedic Nursing. 2006; 25(3): 227-231.
Valaitis RK. Computers and the Internet: Tools for Youth Empowerment. Journal of Medical Internet Research. 2005; 7(5): e51.
Velasco-Garrido M, Busse R, Hisashige A. Are Disease Management Programs Effective in Improving Quality of Care for People with Chronic Conditions? World Health Organization. 2003 Aug; 2-12.
Wilson M. The Future of Telemedicine. Studies of Health Technology and Informatics. 2002; 80:129–136.
Won HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM et al. Establishment of Blood Glucose Monitoring System Using the Internet. Diabetes Care. 2004; 27(2): 478-483.